Popliteal Knee Pain

Popliteal knee pain refers to discomfort or swelling behind the knee, in an area called the popliteal fossa. This region houses key parts of your leg’s movement system, including the popliteus muscle, blood vessels, and nerves that help your knee bend and stay stable.
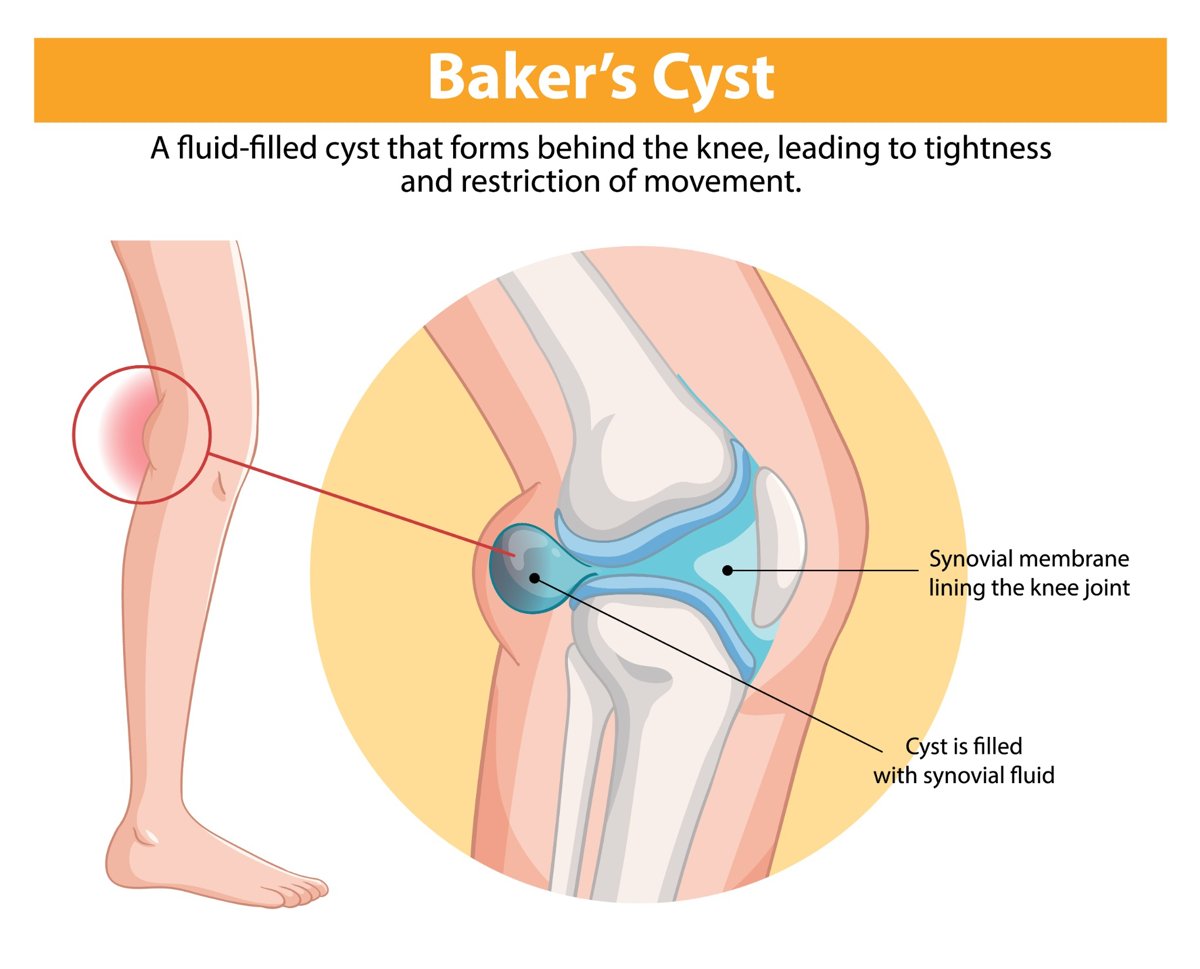
When something goes wrong in this area, it can cause sharp pain, tightness, or a feeling of fullness behind the knee. One common cause is a Baker’s cyst, which often develops along with arthritis or inflammation in the joint.
Common causes of popliteal knee pain include:
- Muscle or tendon strain (such as the popliteus muscle)
- Swelling or fluid buildup (Baker’s cyst)
- Arthritis-related inflammation
- Blood vessel or nerve irritation
Popliteal pain may come on gradually or suddenly, and it can make walking, bending, or standing more difficult. In some cases, a visible lump may form behind the knee.
Recognizing what is behind your popliteal pain is the first step toward relief. Early treatment can reduce swelling, ease discomfort, and help prevent joint damage from progressing, especially if arthritis is involved.
Anatomy of the Popliteal Region
The area behind the knee is called the popliteal fossa. It is bordered by the hamstring muscles above and the calf muscles below. Key structures include:
- Popliteus muscle: A small triangular muscle that runs diagonally across the back of the knee. It “unlocks” the knee by rotating the thigh bone on the shin bone when you begin to bend your leg. The muscle also stabilizes the knee when walking downhill or changing direction.
- Popliteus tendon: Connects the popliteus muscle to the femur. Overuse or sudden twists can cause popliteus tendonitis or strain, leading to sharp pain at the back of the knee.
- Blood vessels and nerves: The popliteal artery and vein, tibial nerve and common fibular nerve pass through this area and supply the lower leg.
Because the popliteal area is crowded with important tissues, swelling or lumps can quickly cause discomfort or limit movement.
What Is a Popliteal (Baker’s) Cyst?
A popliteal cyst—often called a Baker’s cyst—is a fluid‑filled lump at the back of the knee. It forms when excess synovial fluid, the lubricating liquid within the joint, escapes through a weak spot in the joint capsule and collects in a pouch behind the knee.
Baker’s cysts are benign (non‑cancerous) but can cause discomfort.
Popliteal (Baker’s) Cyst Symptoms
- A noticeable bulge or swelling behind the knee
- A feeling of fullness or tightness when bending or straightening the leg
- Knee pain and stiffness
- Swelling that extends into the calf or thigh
Sometimes cysts rupture, releasing fluid into the calf and causing sharp pain and swelling. Ruptured cysts can mimic the symptoms of a blood clot, so seek medical evaluation if you experience sudden calf swelling or redness.
Popliteal (Baker’s) Cyst Causes and Risk Factors
The most common causes of popliteal cysts are knee arthritis and injuries. Arthritis damages cartilage, causing inflammation and the production of excess synovial fluid. The fluid has nowhere to go inside the joint, so it bulges outward into the popliteal space. Knee injuries, especially meniscus tears, can also lead to fluid buildup.
Adults between the ages of 35 and 70, athletes, and individuals whose jobs require heavy knee use are more likely to develop Baker’s cysts. Underlying inflammatory conditions, such as rheumatoid arthritis or gout, are additional risk factors.
Popliteal Problems and Knee Osteoarthritis

When cartilage wears down due to osteoarthritis, the joint surfaces become rough and inflamed. This inflammation triggers the synovial membrane to produce more fluid.
Because the joint capsule cannot expand evenly, fluid is forced out of the back of the knee, forming a cyst. A Baker’s cyst, therefore, is often a warning sign of underlying joint degeneration rather than a problem in isolation. Treating the cyst without addressing the arthritis typically leads to recurrence.
Other popliteal problems include popliteus tendonitis or popliteus muscle strain. Repetitive downhill running or sudden directional changes can strain this small muscle. Symptoms include sharp pain on the outside of the knee joint, particularly when flexing the knee or running downhill. Proper stretching and strengthening of the surrounding muscles usually resolve the issue.
Diagnosing Popliteal Pain
To diagnose the cause of popliteal pain, your healthcare provider will:
- Take your history: Ask about activities, injuries, and associated symptoms like swelling or locking.
- Perform a physical exam: Palpate the back of the knee to assess for lumps, tenderness, or increased warmth. The presence of a visible bulge that fluctuates with knee movement is characteristic of a Baker’s cyst.
- Use imaging tests: Ultrasound can confirm the presence of a cyst and distinguish it from solid masses. MRI may be needed to identify meniscal tears, cartilage damage, or other pathology. An X‑ray helps evaluate joint space narrowing associated with osteoarthritis.
If symptoms suggest a blood clot (deep venous thrombosis), urgent testing is essential to rule out this serious condition.
Popliteal (Baker’s) Cyst Treatment and Management Options

Conservative Measures
- Rest and activity modification: Avoid activities that aggravate swelling, such as prolonged standing or high‑impact sports.
- Ice and compression: Applying ice and using a compression wrap can reduce swelling and pain.
- Elevation: Elevate your leg when resting to facilitate fluid drainage.
- Pain relief: Over‑the‑counter medications like acetaminophen or non‑steroidal anti‑inflammatory drugs (NSAIDs) may relieve pain and inflammation.
Physical Therapy and Strengthening
Strengthening the quadriceps, hamstrings, and calf muscles helps offload the joint and may reduce cyst formation. Stretching tight muscles, especially the hamstrings and calf, can improve mobility. A physical therapist can guide you through safe exercises and monitor your progress. Addressing muscle imbalances also helps prevent popliteus strain.
Medical Management
- Aspiration: Your provider may drain fluid from the cyst using a needle. This relieves pressure but may not prevent fluid from returning.
- Corticosteroid injection: An injection into the knee joint can reduce inflammation, slow fluid production, and shrink the cyst. The effect is usually temporary.
- Treating the underlying cause: Managing osteoarthritis with viscosupplementation, platelet‑rich plasma therapy, or other arthritis treatments often reduces fluid production. Visit our what is osteoarthritis page to learn more about joint degeneration.
Supportive Devices
Wearing a supportive brace may stabilize the knee and reduce strain on the popliteal structures. For patients dealing with osteoarthritis, our fluoroscopy‑guided treatments can ensure precise delivery of injections for more effective relief.
When Surgery Is Necessary for Popliteal

Surgery is rarely needed for Baker’s cysts. However, if the cyst is large, recurrent, or causing nerve or vascular compression, surgical removal may be considered. More commonly, surgery addresses the underlying cause, such as repairing a torn meniscus or removing loose bodies inside the joint. Arthroscopic surgery is less invasive and has a quicker recovery time.
Prevention and Knee Care
- Maintain a healthy weight: Reducing excess pounds reduces stress on your knees and decreases fluid production.
- Exercise regularly: Low‑impact activities like swimming and cycling improve joint health without overloading the knees. Strengthening hip and thigh muscles provides better alignment.
- Warm up and stretch: Proper warm‑up before exercise and stretching after activity protect the popliteus muscle and surrounding tissues.
- Avoid sudden increases in activity: Gradually increase intensity or mileage to prevent overuse injuries.
When to Seek Professional Help
If you notice a lump behind your knee, experience persistent swelling, or have difficulty bending or straightening your knee, see a healthcare professional. Seek immediate care if you develop calf swelling, redness or warmth, as these may indicate a blood clot. Persistent pain after rest or worsening knee function could signal worsening arthritis or another underlying condition that requires treatment.
Arthritis Knee Pain Centers
Popliteal pain and swelling often result from problems inside the knee joint. Whether it’s a popliteus muscle strain, tendonitis or a fluid‑filled Baker’s cyst, treating the underlying issue—often knee arthritis—is essential for lasting relief.
Strengthening muscles, maintaining a healthy weight and using conservative treatments can ease discomfort. If conservative care isn’t enough, targeted injections or surgery may be considered.
To learn more about your options and receive personalized care, schedule your screening with Arthritis Knee Pain Centers.
