How Does the Semimembranosus Muscle Impact Your Knee?
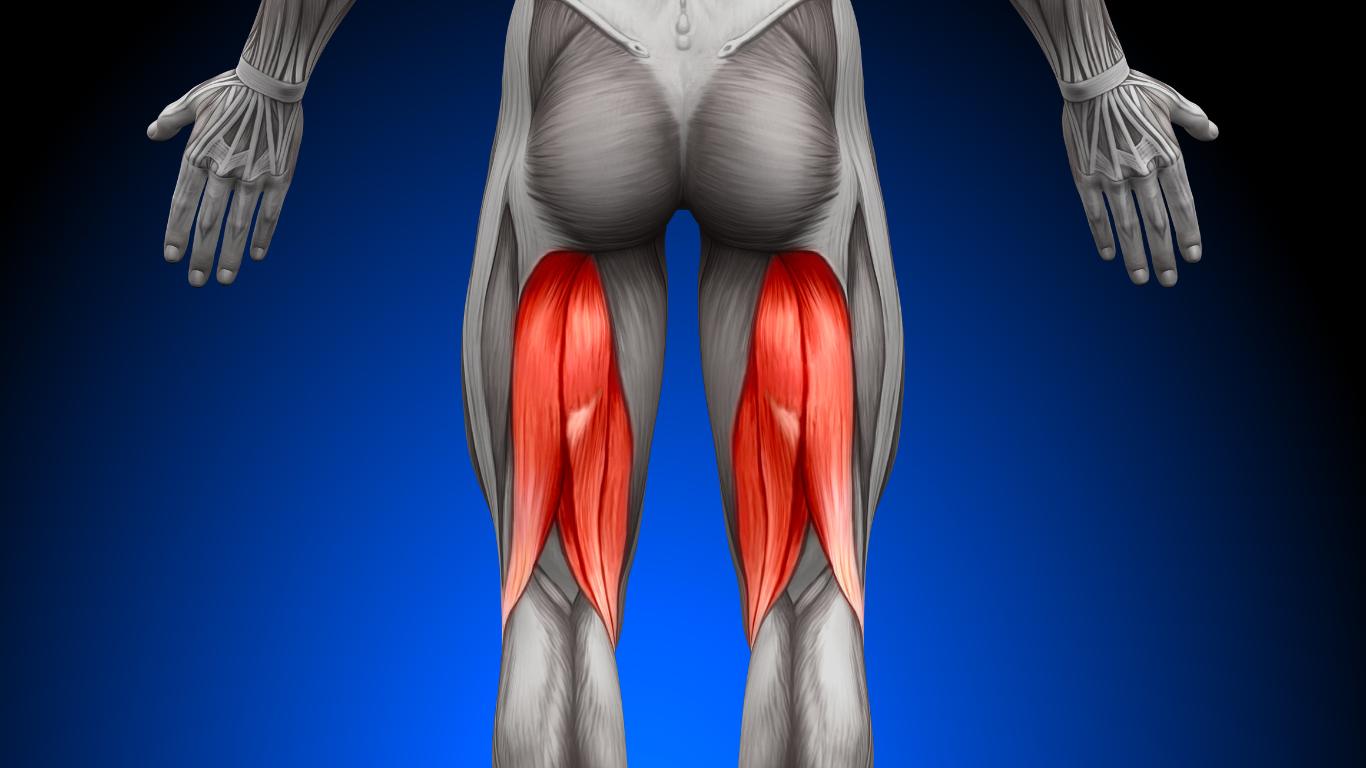
The semimembranosus is one of three hamstring muscles that sit on the back of your thigh. It starts at the ischial tuberosity of the pelvis and runs down the inner part of the thigh to connect to the inside of the tibia, just below the knee.
Since its tendon crosses both the hip and knee joints, it helps with movements like extending your hip, bending your knee, and gently rotating your leg inward. More importantly, it helps stabilize your knee when you walk, climb stairs, or get up from a chair.
This support keeps the knee steady and reduces the risk of it moving in ways it shouldn’t. If the semimembranosus becomes tight, weak, or injured, it can throw off how your leg moves and increase stress on the knee joint.
Over time, this added strain can lead to knee pain and may even speed up the wear and tear that causes knee osteoarthritis. It can also make your leg feel less stable and affect how your other muscles, like your glutes and quadriceps, work together.
Key Ways the Semimembranosus Affects Knee Health:
- Provides stability to the knee during walking, standing, and bending
- Prevents excessive movement that can lead to joint wear over time
- Helps control leg rotation, which protects the knee from twisting injuries
- Supports shock absorption during activities like climbing stairs or rising from a chair
- Works in coordination with nearby muscles to keep knee movement smooth and balanced
- Weakness or tightness in the muscle can increase joint stress and disrupt alignment
Even though it is just one muscle, the semimembranosus plays a big role in helping your knee function properly every day. When it is not doing its job, the effects can add up and lead to pain, instability, and long-term joint problems if not addressed early.
The Semimembranosus at a Glance
Here’s a quick overview of where this muscle sits and what it does:
- Location: Posteromedial thigh, next to the semitendinosus and biceps femoris.
- Origin: Ischial tuberosity of the pelvis.
- Insertion: Medial condyle of the tibia and posterior surface of the knee capsule.
- Actions: Hip extension, knee flexion, internal rotation of the leg, and pelvic stabilization.
The distal tendon has multiple insertion points, including the fascia of the popliteus, the oblique popliteal ligament, and the posteromedial tibia. These attachments allow it to support the back of the knee and work with other hamstrings to control movement. Because of its broad insertion, irritation of the semimembranosus can cause pain along the inner knee and behind the knee.
Why This Muscle Matters for Knee Health
A healthy semimembranosus helps absorb shock and stabilize the knee during gait. When the muscle is weak or inflexible, your knee may track poorly, putting extra stress on cartilage and ligaments. Over time, this can contribute to the development of osteoarthritis.
Studies have shown that the hamstring muscles—especially the semimembranosus—are significantly stiffer in people with knee osteoarthritis compared with healthy controls. Higher muscle stiffness correlates with more pain and poorer knee function.
How Poor Semimembranosus Function Leads to Knee Problems
When this muscle isn’t working properly, several problems can develop:
- Reduced shock absorption: When the muscle can’t absorb forces effectively, more stress passes to cartilage and bones.
- Altered knee mechanics: Tightness may cause the knee to rotate inward, increasing pressure on the joint.
- Tendon irritation: Chronic friction from bone spurs or degenerative meniscal tears can irritate the semimembranosus tendon and the surrounding pes anserine tendon.
- Increased stiffness: Stiffer muscles are associated with higher pain scores and reduced functional ability.
Causes of Semimembranosus Pain
Several factors can injure or irritate this muscle:
- Overuse or sudden loading: Activities like long-distance running, heavy lifting, or sudden sprints can strain the muscle.
- Muscle imbalances: Weak quadriceps or tight hips can overload the hamstrings.
- Poor posture: Prolonged sitting causes hamstrings to tighten and shorten, increasing strain when you stand and walk.
- Aging and osteoarthritis: Degenerative changes in the knee, such as osteophyte formation and meniscal tears, can irritate the tendon.
- Pes anserine bursitis: Inflammation of the bursa where the semitendinosus, gracilis and sartorius insert may mimic semimembranosus pain.
Recognizing the Signs
Tendon problems typically cause pain and stiffness along the back or inner side of the knee. You may notice:
- Tenderness near the posteromedial knee and just below the joint line.
- Pain that worsens when bending the knee, climbing stairs, or stretching your hamstring.
- A snapping sensation or feeling of tightness behind the knee.
- Weakness or instability when trying to straighten the leg.
Because semimembranosus issues can mimic other problems, such as hamstring strains, meniscal tears or sciatica, it’s essential to see a clinician for a proper evaluation. Diagnostic imaging, such as ultrasound or MRI, may be used to confirm tendon irritation or partial tears.
Semimembranosus Tendinopathy and Osteoarthritis
As we age, cartilage in the knee gradually wears down, leading to osteoarthritis. This condition can create friction between the joint structures and the hamstring tendon. Older individuals with degenerative meniscal tears often develop semimembranosus tendinopathy because osteophytes (bone spurs) and joint debris rub against the tendon.
In these cases, the tendon becomes thickened and painful, particularly when walking or bending the knee. Because osteoarthritis is a chronic condition, tendon irritation may come and go with activity levels and flare-ups.
Why Tendinopathy Develops
The semimembranosus tendon runs between the medial head of the gastrocnemius (calf) and the semitendinosus, and it inserts in multiple locations. Friction from these neighboring structures, combined with repetitive eccentric loading (such as descending stairs or lowering into a chair), can cause microtears.
Over time, the tendon degenerates and becomes thicker and less elastic. This degenerative tendinopathy is more common in older adults with osteoarthritis or degenerative meniscal tears.
Preventing Semimembranosus Problems
Keeping your hamstrings strong and flexible is one of the best ways to protect your knees. Try these tips:
- Regular stretching: Perform gentle hamstring stretches by lying on your back and lifting one leg with a strap or towel. Hold for 20–30 seconds and repeat two to three times per leg.
- Strength training: Exercises like bridges, hip hinges and Romanian deadlifts strengthen the hamstrings without overloading the knees.
- Warm up and cool down: Warm muscles are less likely to strain. A brisk walk or gentle cycling for 5–10 minutes before exercise helps prepare your hamstrings.
- Maintain a healthy weight: Excess weight increases the load on your knees. Losing even 5–10 pounds can reduce stress on the joints.
- Use supportive footwear: Choose shoes that cushion your steps and align your legs properly. Avoid high heels or overly worn shoes.
Additional Support for Arthritic Knees
If you already have knee osteoarthritis, supportive aids can ease stress on the tendon:
- Arthritis knee brace: Wearing a properly fitted brace can offload pressure from the medial knee and support hamstrings.
- Viscosupplementation: Hyaluronic acid injections lubricate the joint and may reduce friction on the tendon. Learn more about this option on our viscosupplementation page.
- Genicular artery embolization: This minimally invasive procedure reduces blood flow to painful areas and can decrease chronic knee pain. Discover how it works on our genicular artery embolization page.
- Platelet‑rich plasma (PRP) therapy: Injections using your own platelets promote healing of tendon tissue. Visit our PRP therapy page to learn more.
Treating Semimembranosus Injuries
If you develop semimembranosus tendinopathy or a hamstring strain, early treatment can reduce healing time.
At-Home Care
At home, you can take steps to reduce pain and promote healing:
- Rest and activity modification: Limit activities that cause pain, such as running or deep squats. Opt for low-impact exercises like swimming or cycling.
- Ice therapy: Apply ice packs to the back of the knee for 15–20 minutes several times a day to reduce pain and swelling.
- Compression and elevation: Wrap the knee lightly with an elastic bandage and elevate your leg to decrease swelling.
- Over-the-counter pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can ease discomfort. Always consult your doctor before starting new medications.
Physical Therapy
Physical therapy can improve flexibility and strength, enabling the tendon to heal and reducing recurrence. A therapist will guide you through:
- Stretching exercises for hamstrings, calves, and hips to restore flexibility.
- Strengthening exercises focusing on hamstrings, glutes, and core. Eccentric exercises, where you slowly lower your leg against resistance, are particularly effective for tendinopathy.
- Gait training and posture correction to ensure proper knee alignment.
- Activity progression so you return to normal activity without re-injury.
Medical and Interventional Options
More advanced therapies are available when conservative measures don’t provide enough relief:
- Corticosteroid injections: These provide short-term relief by reducing inflammation. However, repeated injections may weaken tendon tissue, so they should be used sparingly.
- PRP therapy: Using concentrated platelets from your own blood can stimulate healing in chronic tendon injuries.
- Needle tenotomy: A procedure in which a doctor uses a needle to create small holes in the tendon, promoting blood flow and healing.
- Surgery: Rarely needed, surgery may be considered for complete tendon ruptures or chronic pain unresponsive to conservative measures.
When to Seek Medical Help
Consult your healthcare provider if:
- Pain persists for more than a few weeks despite rest and self-care.
- You experience sharp pain or swelling that limits your ability to walk.
- There’s a popping sensation or sudden weakness in the hamstrings.
- You have known knee osteoarthritis, and new symptoms develop.
Early evaluation ensures the correct diagnosis and prevents further damage. Your doctor may order imaging studies to rule out other conditions like meniscal tears or knee arthritis.
Living Well With Knee Osteoarthritis
In addition to caring for your semimembranosus, long-term strategies help manage osteoarthritis:
- Stay active: Aim for 150 minutes of moderate-intensity exercise per week, focusing on low-impact activities. Gentle strength training supports joints.
- Watch your weight: Maintaining a healthy weight reduces knee load and may slow cartilage breakdown.
- Eat anti-inflammatory foods: Focus on fruits, vegetables, fatty fish and whole grains. Avoid excessive sugar, refined carbs and processed foods.
- Consider supplements: Some people find relief with turmeric, omega-3 fatty acids or glucosamine-chondroitin. Always discuss supplements with your doctor.
- Try supportive devices: In addition to braces, cushioned insoles or a cane may reduce knee strain. Check out our post on the best knee brace for pain to see different options.
Exercises to Strengthen and Stretch Your Semimembranosus
To keep your semimembranosus strong and flexible, incorporate these exercises into your routine:
- Seated hamstring stretch: Sit on the edge of a chair with one leg extended forward and heel on the ground. Lean forward from the hips until you feel a gentle stretch in the back of your thigh. Hold for 20–30 seconds and repeat on the other side.
- Bridge with single‑leg extension: Lie on your back with your knees bent. Lift your hips into a bridge, then extend one leg straight while keeping your hips level. Hold briefly, lower and repeat. This exercise strengthens hamstrings and glutes without stressing the knee.
- Standing hip hinge: Stand with your feet hip‑width apart and a slight bend in your knees. Hinge at the hips, pushing your buttocks back while keeping a neutral spine. Return to standing. This trains the hamstrings to lengthen under control.
- Gentle yoga or tai chi: Flowing movements improve flexibility and balance. Poses like downward dog and forward fold stretch the entire posterior chain, including the semimembranosus.
Always listen to your body and stop if you feel sharp pain. If you have significant knee osteoarthritis, consult a physical therapist before starting a new exercise program to ensure movements are safe and adapted to your needs.
Ready to Get Back on Your Feet?
Your semimembranosus may be a small muscle, but its role in knee stability is significant. Keeping it flexible and strong helps protect your knees and may slow the progression of osteoarthritis.
If you’re experiencing knee pain, don’t ignore it. A personalized evaluation can pinpoint whether the semimembranosus or another structure is causing your discomfort.
Our team at Arthritis Knee Pain Centers specializes in non‑surgical, image-guided treatments like viscosupplementation, platelet-rich plasma therapy and genicular artery embolization that target the root causes of knee pain and help you stay active. Take the first step toward relief and schedule a no-charge, no-obligation screening today.
